Genetics and genomics for midwifery practice v2
| Site: | Royal College of Midwives |
| Course: | Sample course (extract from Genetics and genomics) |
| Book: | Genetics and genomics for midwifery practice v2 |
| Printed by: | Guest user |
| Date: | Thursday, 18 April 2024, 5:49 PM |
1. Genetics and genomics - the basics
 This module on Genetics and genomics for midwifery practice has been written for i-learn by the National Genetics Education and Development Centre and revised by Dr Simon Hettle, Lecturer in Biomedical Science and Genetic Modification Safety Officer at the University of the West of Scotland. It has been designed to help midwives develop a better understanding of genetics and genomics.
This module on Genetics and genomics for midwifery practice has been written for i-learn by the National Genetics Education and Development Centre and revised by Dr Simon Hettle, Lecturer in Biomedical Science and Genetic Modification Safety Officer at the University of the West of Scotland. It has been designed to help midwives develop a better understanding of genetics and genomics.
Completion of this module will enable you to:
- understand your role in genetics and genomics
- refresh and/or enhance your knowledge
- consider the skills required to gain appropriate information from the families in your care
- reflect on various situations you might encounter in practice when these skills and knowledge will be required
1.1. Learning objectives
By the end of this session you should be able to:
- Demonstrate a knowledge of how genetic conditions occur and how they may be inherited within a family
- Describe your role in identifying those with a higher probability of having a genetic condition and how you would refer to specialist genetic services
- Appreciate how the use of genomic information is likely to impact on maternity care
The session assumes a basic level of knowledge about what genes are, how they work and basic definitions. It may be advisable to refresh your knowledge of the basics. Visit the Health Education England’s Genomics Education Programme website to review:
- Genes and inheritance
- Inheritance of genetic material
- What causes genetic conditions?
You may wish to consult the Genomics glossary.
1.2. Using i-folio to support your learning
 i-folio is the RCM’s e-portfolio that members can access from anywhere providing they have Internet access. As you work through this course you can make notes in i-folio for future reference and use the i-folio reflective journal to reflect on your learning. Click the link for more information on using i-folio to support your learning.
i-folio is the RCM’s e-portfolio that members can access from anywhere providing they have Internet access. As you work through this course you can make notes in i-folio for future reference and use the i-folio reflective journal to reflect on your learning. Click the link for more information on using i-folio to support your learning.
2. Why is understanding genetics and genomics important for a midwife?
 In your role as a midwife, a knowledge of genetics and inheritance is relevant throughout your practice, for example, when following a specialist care plan during delivery and examining and caring for a newborn. However, undertaking initial assessments in the early antenatal period is when most information gathering, recording and interpretation occur.
In your role as a midwife, a knowledge of genetics and inheritance is relevant throughout your practice, for example, when following a specialist care plan during delivery and examining and caring for a newborn. However, undertaking initial assessments in the early antenatal period is when most information gathering, recording and interpretation occur.
It is important to recognise individuals and families who have inherited conditions because their family members may be at an increased chance of developing the condition or of being a carrier. Some conditions are caused by chromosome anomalies and modern techniques can help us to understand their clinical implications. Other conditions are due to a combination of genetic changes which predispose a person to a condition. So, a midwife’s understanding of genetics and inheritance is important for the fetus, the mother and the wider family.
Genomic information is increasingly being used to understand the underlying basis of disease, to refine diagnoses, target treatment and diagnose infections. Midwives may therefore see families where previously unknown genetic disease has been identified, or where the cause of multiple fetal anomalies has been shown to be due to problems with several genes.
3. Where will you encounter genetics in your practice?
A significant part of the midwife’s role is recognising potential concerns, including recognition of families with, or with a potential to have, a genetic condition. As a midwife, you form good working relationships with women and their families and have unique opportunities to assist women and help them achieve the best outcome from their pregnancy.
As face-to-face time with women is limited, your skills of questioning and listening, together with a good working knowledge of genetics and genomics, will enable you to accurately assess families and be alerted to the possible presence of a genetic condition.
Once alerted to a potential genetic problem or risk, it is your responsibility to take appropriate action.
You may encounter genetics in your practice when caring for women in the antenatal, delivery or postnatal periods.
Question: When would you suspect that there could be a link to a genetic problem or a need for midwives to have knowledge of genomics? Select ALL of the following options that you believe to be correct.
|
|
3.1. What might alert you?
At the booking clinic you will ask about conditions in the family. Sometimes, a known condition will confirm a mode of inheritance (such as cystic fibrosis). In other cases, the pattern of people with the condition may indicate the need for referral to determine if there is a strong genetic component.
Clinical clues suggesting that a condition has a strong genetic component include the following:
- An individual or a couple with three or more pregnancy losses (miscarriages or stillbirths)
- Multiple congenital anomalies or dysmorphic features, particularly if associated with developmental delay
- Multiple closely-related individuals with the same condition, particularly if the condition is rare
- Medical problems in the offspring of parents who are related by blood
- Disorders which occur at an earlier age than usual (especially if onset is early in multiple family members)
- Congenital or juvenile deafness
- Congenital or juvenile blindness
- Sudden cardiac deaths in people who seemed healthy
3.2. What is genetic material?
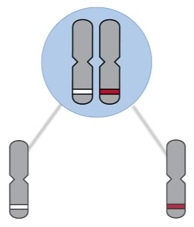
Humans have about 23,000 genes, which are arranged in linear order on chromosomes. Each chromosome is one long molecule of DNA and contains hundreds of genes.
The bulk of a cell’s DNA is found in its nucleus and, together with the DNA in the mitochondria, this genetic material is the human genome.

3.3. What causes genetic conditions?
Click each set of images for different conditions to learn more about each type:
Three scenarios follow which will give you the opportunity to reflect on your role and your knowledge of the inheritance patterns of the conditions discussed and the implications for pregnancy and the family.
4. Alex's Story
 You are a community midwife undertaking an initial assessment with Alex, a primigravida who is 12 weeks pregnant, at her home.
You are a community midwife undertaking an initial assessment with Alex, a primigravida who is 12 weeks pregnant, at her home.
Although Alex was born in the UK, her family has a Mediterranean background. Alex’s partner has lived in the UK for many years but was born in Greece. Both are fit and well and very much looking forward to becoming parents.
You know that with their population ancestry there is a possibility that the couple may be carriers for beta-thalassaemia and, if so, their baby could inherit the condition.
4.1. Alex's story 2
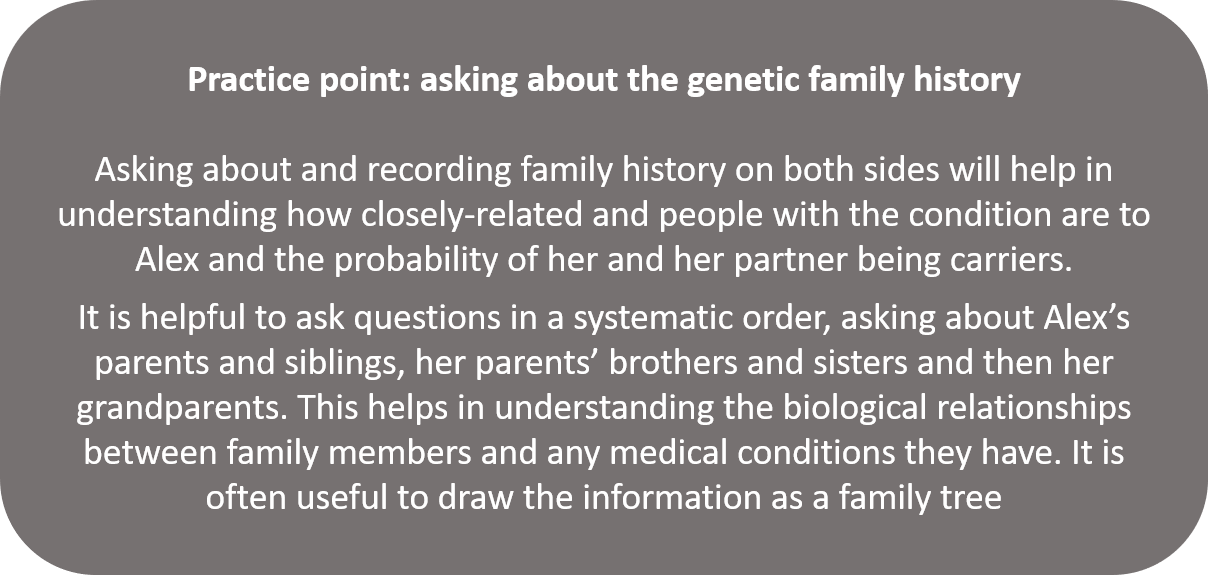
You discuss with Alex that because being a carrier for beta-thalassaemia is common amongst people of her and her partner’s population ancestry. They could be carriers for beta-thalassaemia even if no one in their families is known to have the condition.
You also explain that you need to ask if anyone in the family has beta-thalassaemia as this would increase the chance of being a carrier.
4.2. Alex's story 3
Alex has heard about beta-thalassaemia because she thinks someone in her family has the condition. She would need to check with her aunt in Greece, she cannot ask her parents as they both died in a road traffic accident.
She knows she has not been tested herself. She doesn’t think her partner has any relatives with beta-thalassaemia.
What actions will you take at this point? Tick the options and then click the feedback button for further information.
| Record your findings on the handheld record, stating that it is possible that both partners may be carriers because of population ancestry and there may be evidence of beta-thalassaemia on one side of the family. | |
| Record that you have advised Alex that there is a possibility of her and her partner being carriers and if this is confirmed there is a possibility that they may have a baby with beta-thalassaemia. | |
| Advise Alex to mention the condition to the antenatal clinic midwife when she visits the hospital later in the month and she will deal with it. | |
| Discuss Alex's case with the screening midwife or consultant at the obstetric unit and arrange an appointment for Alex and her partner. | |
| Ask Alex to let you know the information she finds out from her family and her partner as soon as possible. | |
4.3. Alex's story 4
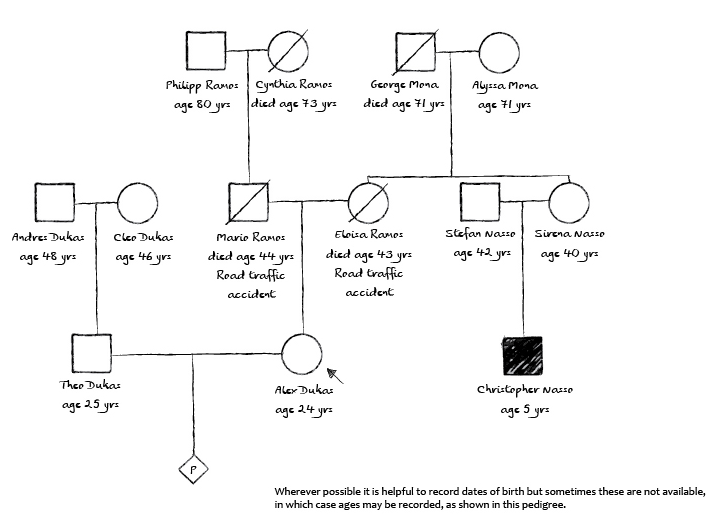
Alex and her partner went to see the screening midwife. Alex had found out more information about her family. Her aunt, her mother’s sister, has a son who is being treated for beta-thalassaemia. Also, Alex’s partner says that he thought someone had a blood disorder in the family, but that is all he knows.
An understanding of how beta-thalassaemia is inherited and the relationships of people in the family can be used to work out whether someone is likely to be a carrier.
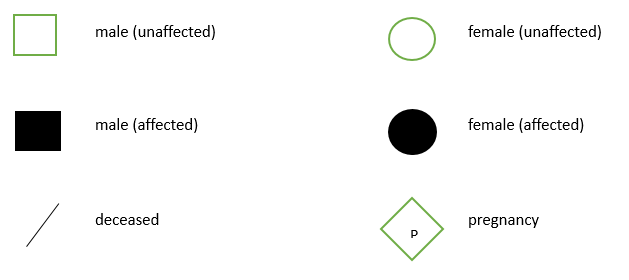
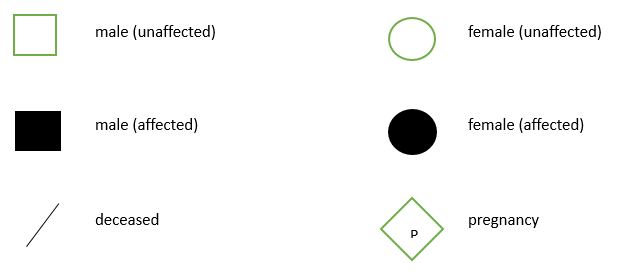
This information is drawn here as a family tree. On the right is a key to the symbols used.
 |
 |
Beta-thalassaemia is an autosomal recessive condition and the next page explains this mode of inheritance.
5. Self-Assessment Quiz
Now answer the questions in this link to the Self-Assessment Quiz Example Questions. You will need to get 75% in order to pass the quiz and obtain a certificate of completion.